Penicillins
What are Penicillins?
Penicillins are a type of antibiotic derived from Penicillium fungi. An antibiotic is a type of medicine that inhibits the growth of, or kills, bacteria.
Penicillin G (also called benzylpenicillin) was discovered by accident in 1928. Alexander Fleming, a Scottish physician-scientist was growing a type of bacteria called Staphylococcus aureus on an uncovered petri dish when it became contaminated with mold spores. He observed that the areas of bacteria near the mold were dying. He isolated the substance from the mold that was killing the bacteria and called it penicillin.
Another naturally occurring penicillin, penicillin V, was later isolated from the same mold. All other penicillins are semi-synthetic (made by modifying the structure of the original naturally occurring penicillins). Modification extends their spectrum of activity, allows them to be taken orally, and increases their resistance against penicillinase, an enzyme produced by some bacteria that inactivates penicillin.
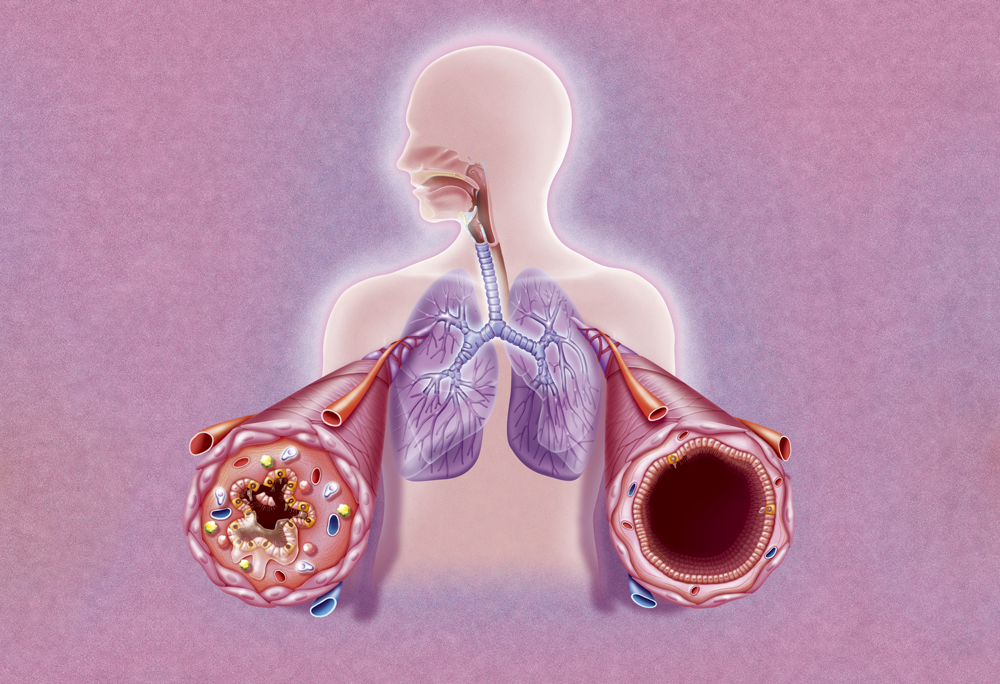
Penicillins work by preventing the cross linking of amino acid chains in the bacterial cell wall. This does not affect pre-existing bacteria, but newly produced bacterial cells have weak cell walls that easily rupture.

Penicillin is a class of antibiotic medications. Penicillins treat bacterial infections like strep throat, ear infections and urinary tract infections. They work by attaching to and damaging the cell walls of bacteria. Types of penicillin include penicillin V, penicillin G, amoxicillin and ampicillin.
What are the differences between penicillins?
The natural penicillins (penicillin G and penicillin V) are only active against gram-positive bacteria (see below for an explanation). Penicillin V is more acid-resistant than penicillin G, which means it can be taken orally.
Modern semi-synthetic penicillins include ampicillin, carbenicillin (discontinued), and oxacillin. These can be taken orally, have some degree of resistance to beta lactamase, and are effective against some gram-negative bacteria. Most bacteria can be classified as gram-positive or gram-negative based on differences in their cell wall structure, which can be distinguished under a microscope using a type of dye. One of the most important differences between these two types of bacteria is that gram-positive bacteria are more susceptible to antibiotics while gram-negative bacteria are more resistant to antibiotics.
Antipseudomonal penicillins, such as piperacillin and ticarcillin (discontinued) are penicillins that have additional activity against some hard-to-kill types of gram-negative bacteria such as Pseudomonas, Enterococcus and Klebsiella. They are useful for urinary tract infections caused by susceptible bacteria because they concentrate in the urine.
Some penicillins are combined with a beta-lactamase inhibitor. A beta-lactamase inhibitor blocks the activity of beta-lactamase enzymes but tends to have little antibiotic activity on its own. Some penicillins (such as oxacillin, dicloxacillin, and nafcillin) are naturally resistant to certain beta-lactamases and are called penicillinase-resistant penicillins. Others, such as amoxicillin, ampicillin, and piperacillin can have their activity extended by combining them with a beta-lactamase inhibitor. Clavulanate, sulbactam, and tazobactam are all beta-lactamase inhibitors.
Are penicillins safe?
Penicillins are generally safe, with low toxicity and good efficacy against susceptible bacteria.
Many people believe that they are allergic to penicillin. However, true penicillin allergy is rare, and only occurs in 0.01-0.05% of people who take penicillin. Symptoms may include nausea, vomiting, itchy skin, rash, wheezing, swelling around the throat, and respiratory collapse.
What are the side effects of penicillins?
Penicillins generally cause few side effects. The most common side effects reported include abdominal pain, headache, rash, diarrhea, and taste perversion.
Penicillins may cause anaphylaxis in those allergic to penicillin, but the overall incidence of anaphylaxis is rare (0.01-0.05%).
Rarely, some people may develop a super-infection due to overgrowth of a naturally occurring bacterium called Clostridium difficile, following use of any antibiotic, including penicillins. Symptoms may include severe diarrhea.
Uncommonly, an overgrowth of the yeast, Candida albicans, may occur following penicillin use, resulting in the symptoms of thrush.
Antibiotics in the penicillin class are among the most commonly prescribed antibiotics. They include many individual medications, such as penicillin G, amoxicillin, nafcillin, oxacillin, dicloxacillin, flucloxacillin, ampicillin, and piperacillin-tazobactam.
Penicillin’s mechanism of action
Penicillin and other antibiotics in the beta-lactam family contain a characteristic four-membered beta-lactam ring. Penicillin kills bacteria through binding of the beta-lactam ring to DD-transpeptidase, inhibiting its cross-linking activity and preventing new cell wall formation.
Today, penicillin, considered the first wonder drug, is used to treat throat infections, meningitis, syphilis and other bacterial infections. It works by inhibiting enzymes involved in building bacterial cell walls and by activating other enzymes that break these protective barriers down.
Sulphonamides are an important class of antibiotic drugs with a wide range of activity, being very effective against gram-positive and certain gram-negative bacteria (White and Cooper 2003).
The penicillin family of antibiotics contains over 15 chemically related drugs (e.g. penicillin, ampicillin, amoxicillin, amoxicillin-clavulanate, methicillin) that are given by mouth or injection for the treatment of many bacterial infections. It is one of the most frequently used classes of antibiotics in the world.
Penicillium mold naturally produces the antibiotic penicillin. 2. Scientists learned to grow Penicillium mold in deep fermentation tanks by adding a kind of sugar and other ingredients.
Common penicillins available in the U.S.
Aminopenicillins
Spectrum of activity:
- Most gram-positive bacteria, some gram-negative bacteria (such as E. coli and H. influenzae).
| Generic name | Brand name examples |
|---|---|
| amoxicillin | Amoxil, Moxatag |
| ampicillin | Generic only |
Antipseudomonal penicillins
Spectrum of activity:
- Most gram-positive and gram-negative bacteria
- Antipseudomonal and antiprotozoal activity
- Usually given with a beta lactamase.
| Generic name | Brand name examples |
|---|---|
| piperacillin | Generic only |
Beta-lactamase inhibitors
Spectrum of activity:
- Effective against most gram-positive and gram-negative bacteria including those that produce beta-lactamases (eg, bacteroides sp., enterococcus sp., staphylococcus sp.)
| Generic name | Brand name examples |
|---|---|
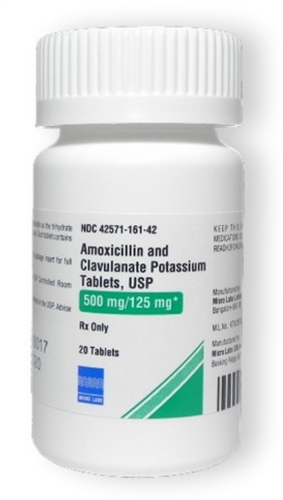
| amoxicillin/clavulanate | Augmentin, Amoclan |
| ampicillin/sulbactam | Unasyn |
| piperacillin/tazobactam | Zosyn |
Natural penicillins
Spectrum of activity:
- Effective against most gram-positive bacteria and a limited number of gram-negative bacteria.
| Generic name | Brand name examples |
|---|---|
| penicillin g benzathine | Bicillin L-A |
| penicillin v | Penicillin VK |
Penicillinase-resistant penicillins
Spectrum of activity:
- Effective against most gram-positive and gram-negative bacteria
- Naturally resistant to beta-lactamase.
| Generic name | Brand name examples |
|---|---|
| dicloxacillin | Dycill |
| nafcillin | Generic only |
| oxacillin | Generic only |
Medical conditions that need Penicillins
Penicillins may be used to treat a wide range of infections caused by susceptible bacteria, such as: