Pronunciation: key-true-duh
Generic name: pembrolizumab
Dosage form: solution for intravenous infusion
Drug class: Anti-PD-1 and PD-L1 monoclonal antibodies (immune checkpoint inhibitors)
What is Keytruda?
Keytruda is used to treat multiple types of cancer such as melanoma, non-small cell lung cancer, head and neck squamous cell carcinoma, Hodgkin Lymphoma, urothelial carcinoma, gastric cancer, and many others. It is given as an infusion into your vein (IV infusion) every 3 to 6 weeks depending on the type of cancer you have.
Keytruda (pembrolizumab) is an immunotherapy treatment, not chemotherapy, although it is often used with other medicines, including chemotherapy. It works by enhancing the body’s natural immune response against cancer cells.
Keytruda infusion first gained FDA approval on September 4, 2014.
Types of cancer treated with Keytruda
Keytruda is FDA-approved to treat numerous cancers, including certain types of:
- Biliary tract cancer
- Certain types of colorectal cancer
- Cervical cancer
- Classical Hodgkin Lymphoma
- Cutaneous squamous cell carcinoma (cSCC)
- Endometrial cancer
- Esophageal cancer
- Gastric cancer
- Head and neck squamous cell cancer (HNSCC)
- Kidney cancer (renal cell carcinoma)
- Liver cancer (Hepatocellular carcinoma [HCC]) secondary to hepatitis B
- Malignant pleural mesothelioma (MPM)
- Melanoma
- Merkel cell carcinoma (MCC)
- Microsatellite instability-high (MSI-H) or mismatch repair deficient cancers
- Non-small cell lung cancer (NSCLC)
- Primary Mediastinal Large B-cell lymphoma (PMBCL)
- Triple-negative breast cancer
- Tumor mutational burden-high (TMB-H) cancer
- Urothelial cancer including some types of Bacillus Calmette-Guerin (BCG)-unresponsive urothelial cancers.
Some cancers may need to be tested for genetic markers such as PD-L1, dMMR, TMB, or pMMR to determine if Keytruda is right for you.
Note that this is just a summary, see the Keytruda Prescribing Information for specific criteria and prior treatment requirements that may apply for each indication.
Mechanism
Keytruda works through a sophisticated mechanism of action called immune checkpoint inhibition:
- It blocks the PD-1 protein found on T cells
- This prevents PD-1 from interacting with PD-L1 on cancer cells
- This inhibition “takes the brakes off” the immune system, allowing T cells to recognize and attack cancer cells more effectively
- Keytruda enhances the immune system response against cancer.
Keytruda belongs to the drug class called immune checkpoint inhibitors and may also be called a monoclonal antibody.
Clinical trials have shown most people respond to Keytruda within 2-4 months of starting treatment .
Keytruda side effects
The most common side effects of Keytruda when it is used alone are:
- fatigue or excessive tiredness
- pain, including pain in the stomach, muscles, bones, or joints
- rash or itching
- diarrhea
- fever
- cough
- decreased appetite
- shortness of breath
- constipation
- nausea
- low levels of thyroid hormone.
Clinical trials have reported Keytruda side effects that are more common in children than adults are:
- fever
- vomiting
- headache
- stomach area pain
- low levels of white blood cells.
The most common side effects of Keytruda when it is used in combination with chemotherapy or radiotherapy treatments include:
- fatigue or excessive tiredness
- nausea
- constipation
- diarrhea
- decreased appetite
- rash
- vomiting
- cough
- trouble breathing
- fever
- hair loss
- inflammation of the nerves that may cause pain
- weakness and paralysis in the arms and legs
- swelling of the lining of the mouth, nose, eyes, throat, intestines, or vagina
- mouth sores
- headache
- weight loss
- stomach-area (abdominal), joint, or muscle pain,
- trouble sleeping
- bleeding
- blisters, or rash on the palms of your hands and soles of your feet
- urinary tract infection
- low levels of thyroid hormone.
- nausea, vomiting, stomach pain, loss of appetite, diarrhea, constipation, weight loss
- low blood sodium levels, abnormal thyroid, liver and kidney function tests
- low blood cell counts
- tingling or numbness in your hands or feet, loss of movement in the arms and legs
- bleeding
- pain and burning when you urinate
- fever, headache, feeling weak or tired, dizziness, trouble sleeping
- cough, hoarse voice, feeling short of breath
- changes in your sense of taste, dry skin, and dry eyes
- itching, hair loss, rash, or blisters on your hands or feet
- increased blood pressure
- pain in your muscles, bones, or joints
- mouth sores or swelling around your mouth, nose, eyes, throat, intestines, or vagina
- tingling or numbness in your arms or legs.
Prompt medical attention to these side effects is crucial. Your doctor will monitor you during Keytruda treatment.
Serious side effects and warnings
Keytruda is a medicine that works with your immune system to treat certain cancers. Keytruda can cause your immune system to attack normal organs and tissues in any area of your body and can cause serious side effects.
- These problems can sometimes become severe or life-threatening and can lead to death. You can have more than one of these problems at the same time.
- These problems may happen anytime during treatment or even after your treatment has ended
Call or see your healthcare provider right away if you develop any new or worsening signs or symptoms, including:
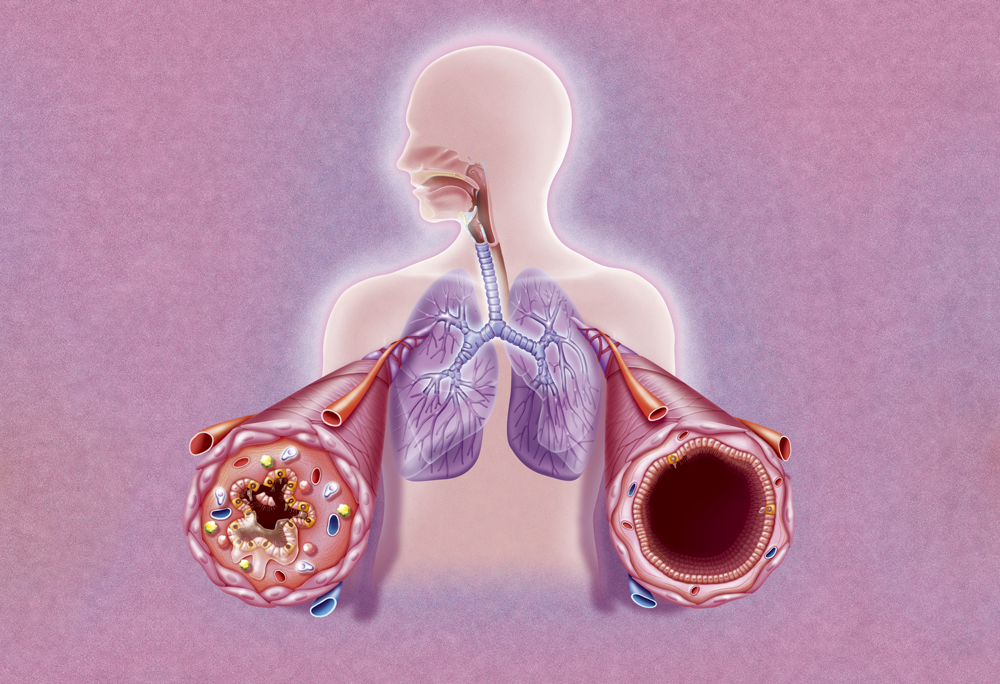
- Lung problems, such as cough, shortness of breath, or chest pain
- Intestinal problems, such as:
- diarrhea (loose stools) or more frequent bowel movements than usual
- stools that are black, tarry, sticky, or have blood or mucus
- severe stomach-area (abdomen) pain or tenderness.
- Liver problems such as
- yellowing of your skin or the whites of your eyes
- dark urine (tea colored)
- severe nausea or vomiting
- bleeding or bruising more easily than normal
- pain on the right side of your stomach area (abdomen).
- Hormone gland problems, such as
- headaches that will not go away or unusual headaches
- urinating more often than usual
- eye sensitivity to light
- hair loss
- eye problems feeling cold
- rapid heartbeat
- constipation
- increased sweating
- your voice gets deeper
- extreme tiredness
- dizziness or fainting
- weight gain or weight loss
- changes in mood or behavior, such as decreased sex drive, irritability, or forgetfulness
- feeling more hungry or thirsty than usual.
- Kidney problems, such as
- decrease in your amount of urine
- swelling of your ankles
- blood in your urine
- loss of appetite.
- Skin problems, such as
- rash
- painful sores or ulcers in your mouth or your nose, throat, or genital area
- itching
- fever or flu-like symptoms
- skin blistering or peeling
- swollen lymph nodes.
- any new or worsening signs or symptoms in other organs, which may include:
- chest pain, irregular heartbeat, shortness of breath, swelling of ankles
- confusion, sleepiness, memory problems, changes in mood or behavior, stiff neck, balance problems, tingling or
- numbness of the arms or legs
- double vision, blurry vision, sensitivity to light, eye pain, changes in eyesight
- persistent or severe muscle pain or weakness, muscle cramps
- low red blood cells, and bruising.
- Infusion reactions can sometimes be severe or life-threatening. Signs and symptoms may include:
- chills or shaking dizziness
- itching or rash
- feeling like passing out
- flushing
- fever
- shortness of breath or wheezing
- back pain.
For people who have had an organ transplant, Keytruda may cause rejection of a transplanted organ or tissue. Your healthcare provider should tell you what signs and symptoms you should report and monitor you depending on the type of organ or tissue transplant that you have had.
Complications, including graft-versus-host-disease (GVHD), in people who have received a bone marrow (stem cell) transplant that uses donor stem cells (allogeneic). These complications can be serious and can lead to death.
- These complications may happen if you underwent transplantation either before or after being treated with Keytruda.
- Your healthcare provider will monitor you for these complications.
Get emergency medical help if you have signs of an allergic reaction to Keytruda (hives, difficulty breathing, swelling in your face or throat) or a severe skin reaction (fever, sore throat, burning eyes, skin pain, red or purple skin rash with blistering and peeling).
Keytruda may cause harm to an unborn baby. Females of reproductive potential should use effective contraception.
Getting medical treatment right away for these side effects may help keep these problems from becoming more serious. This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to the FDA .
Before taking this medicine
To make sure Keytruda is safe for you, tell your doctor if you have:
- an autoimmune disorder such as rheumatoid arthritis, Crohn’s disease, ulcerative colitis, lupus, or psoriasis
- received or plan to receive a stem cell transplant that uses donor stem cells
- had an organ transplant
- had radiation to your chest
- a condition that affects your nervous system such as myasthenia gravis or Guillain-Barré syndrome
- are pregnant or plan to become pregnant
- are breastfeeding.
Pregnancy
Keytruda may harm an unborn baby. Your healthcare provider will give you a pregnancy test to make sure you are not pregnant. Use effective birth control while using Keytruda and for at least 4 months after your last dose. Tell your healthcare provider right away if you think you may be pregnant or if you become pregnant during
treatment with Keytruda.
Breastfeeding
It is not known if Keytruda passes into breast milk. Do not breastfeed while using this medicine and for at least 4 months after your last dose.
How is Keytruda administered?
Keytruda is administered as an infusion into your vein through an intravenous line over 30 minutes.
- In adults, a Keytruda infusion is usually given every 3 weeks or 6 weeks depending on the cancer type being treated and your dosage.
- In children, Keytruda is usually given every 3 weeks.
- Your healthcare provider will decide how many treatments you need.
- Your healthcare provider will do blood tests to check you for side effects.
- If you miss any appointments, call your healthcare provider as soon as possible to reschedule your appointment.
You will need frequent medical tests to help your doctor determine if you are tolerating Keytruda. Do not miss any follow-up visits.
What happens if I miss a dose?
Call your doctor for instructions if you miss an appointment for your Keytruda infusion.
What happens if I overdose?
In a medical setting, an overdose would be treated quickly.
What should I avoid while receiving Keytruda?
Follow your doctor’s instructions about any restrictions on food, beverages, or activity.